TMJ Disorder: Symptoms, Treatments & More
Jaw pain or clicking? We’ll explore TMJ disorder, its symptoms, causes, and treatment options to help you find relief and regain comfort.

TMJ disorder affects millions of people, yet many don't know what's causing their pain. Learning about this condition can lead to faster diagnosis and more effective treatment.
Understanding TMJ Disorder
Jaw pain can significantly impact various aspects of daily life, from eating meals to getting a good night's sleep. Learning what's happening in your jaw joint is the first step toward feeling better.
What is the Temporomandibular Joint (TMJ)?
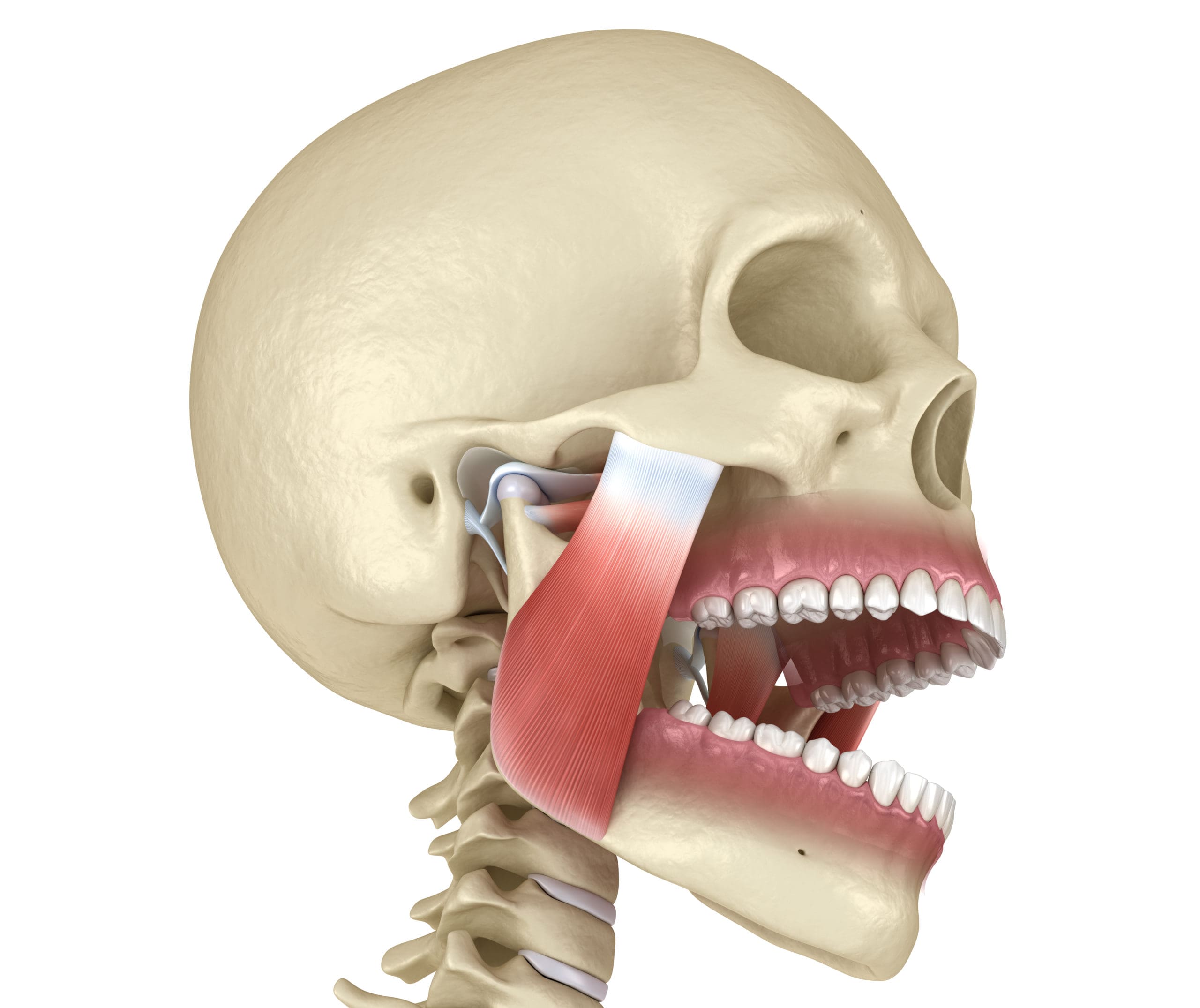
The temporomandibular joint connects your lower jaw to your skull's temporal bone, sitting just in front of each ear. This joint allows you to chew, speak, yawn, and swallow. Unlike simple joints, the TMJ both hinges and slides, making it one of the most complex joints in your body.
This joint gets used more than most people realize. It moves about 2,000 times each day when you talk, eat, and make facial expressions. Though built to last, it can develop problems because of its complex structure and constant use.
What is TMJ Disorder (TMD)?
TMJ disorder, also called temporomandibular disorder (TMD), includes various conditions affecting the jaw joint and surrounding muscles. It's not one single disease but a group of problems causing pain and limited jaw function, which explains why treatments can vary so much. Symptoms range from occasional discomfort to pain that interferes with daily activities.
Many people incorrectly say "TMJ" when referring to the disorder, but TMJ actually means the joint itself. The correct term for the condition is TMD or TMJ disorder.
Who is Most at Risk?
Knowing risk factors helps identify who might benefit from early care. While you can't change some risk factors, knowing your personal risks can help you seek help sooner.
TMJ disorder affects about 5-12% of people in the UK, with women experiencing it more often than men. Women are about twice as likely to develop TMD, especially during their reproductive years. Most cases occur in adults between 20 and 40 years old, though it can affect people of any age.
Symptoms of TMJ Disorder
Noticing TMJ symptoms early can improve treatment results. Many symptoms overlap with other conditions, making TMJ disorders hard to identify. Pay attention to patterns: symptoms that get worse with jaw movement or after stressful times often point to TMJ problems.
Common Symptoms
The main symptoms of TMJ disorder typically involve the jaw and nearby areas. These symptoms may come and go, change in intensity, or affect different places at different times.
- Jaw pain or tenderness: Pain in and around the jaw joint, sometimes spreading to the face, neck, or shoulders
- Clicking, popping, or grinding noises: Sounds when opening or closing your mouth (affects 45-55% of cases)
- Difficulty opening or closing the mouth fully: Limited jaw movement (normal range is 35-55mm)
- Headaches: Often tension-type headaches, with pain in the temples or forehead (affects 70-80% of patients)
- Earaches or ear pain: Aching around the ears without any infection (reported by 50% of patients)
- Locking of the jaw: The jaw may temporarily lock in an open or closed position
- Pain while chewing or talking: Discomfort that increases with jaw use
Less Obvious Symptoms
These additional symptoms often lead people to see doctors other than dentists, delaying proper TMJ diagnosis. Many patients are surprised to learn these seemingly unrelated issues connect to their jaw function.
- Dizziness or vertigo: Reported in 10-15% of cases
- Neck and shoulder pain: Often due to changes in posture to compensate for jaw pain (affects 50% of patients)
- Tinnitus (ringing in the ears): Due to the TMJ's location near ear structures (30-40% of cases)
- Tooth sensitivity: Often resulting from grinding or clenching
- Bite changes: Feeling that teeth don't fit together properly (reported in 25-30% of cases)

Is Jaw Clicking Normal or a Problem?
Joint sounds can be confusing, and many people have them without pain and wonder if they should be concerned. Knowing the difference between harmless clicking and problematic sounds can help you decide when to seek care.
Occasional, painless clicking during wide jaw movements is fairly common and often harmless, affecting 20-30% of people. However, clicking becomes concerning when it is accompanied by pain, locking, or limited movement. Persistent or worsening clicking should be checked by a dental professional.
When to Seek Help
Knowing when to see a professional can prevent unnecessary pain and complications. While minor discomfort might go away on its own, certain signs indicate you need professional evaluation.
See a dentist or doctor if symptoms last more than a week, get worse with jaw use, or interfere with daily activities like eating or speaking. Early care typically leads to simpler treatment and better outcomes.
What Specialists Handle TMJ Disorder?
TMJ disorders often fall between medical and dental care. Knowing which specialists treat these conditions helps navigate the healthcare system more effectively, especially in the UK, where referral pathways can sometimes be complex.
- Dentists: Primary providers for diagnosis and treatment with splints
- Oral Surgeons: For severe cases requiring injections or surgery
- ENT Doctors: To rule out ear-related conditions
- Physical Therapists: For muscle-related TMD treatment
- Pain Specialists: For chronic pain management approaches

Causes and Triggers
Understanding what causes TMJ disorders helps target treatment effectively. While you can't avoid some causes (like genetics or certain medical conditions), many triggers can be changed or eliminated. Identifying your specific triggers is often key to managing symptoms.
Primary Causes
TMJ disorders rarely have just one cause; most cases result from several factors creating conditions for dysfunction. This explains why treatment often needs to address multiple aspects at once.
- Joint and Muscle Issues:
- Disk displacement: The cushioning disk moves out of position
- Arthritis: Osteoarthritis or rheumatoid arthritis affecting the TMJ
- Muscle spasms: Overuse or tension in jaw muscles
- Injury or Trauma:
- Direct trauma from accidents or impacts
- Microtrauma from habits like excessive gum chewing or nail biting
- Behavioral and Lifestyle Factors:
- Bruxism: Teeth grinding or clenching, often related to stress
- Poor posture: Forward head posture increases tension in neck and jaw muscles
- Dietary habits: Chewing tough foods or excessive gum chewing
Can Stress or Anxiety Make It Worse?
Yes, stress and anxiety significantly impact TMJ disorder. They trigger unconscious jaw clenching or grinding, increasing muscle tension and joint strain. Chronic stress makes pain sensitivity worse, creating a cycle where TMJ pain causes more stress, which then worsens the TMJ symptoms.
Today's high-stress environment makes this connection particularly relevant for London residents balancing demanding jobs, commuting, and busy social lives.
Why is poor posture linked to TMJ issues?
The increase in desk work and mobile device use has led to widespread poor posture, affecting jaw health.
Poor posture, especially forward head posture, common in desk workers, is linked to TMJ problems. When your head sits forward, it strains the neck and jaw muscles, altering how the TMJ functions. UK studies found that improving workplace ergonomics reduced TMJ symptoms by 30% in office workers.
Can Dental Problems Contribute to TMJ Disorder?
The relationship between dental issues and TMJ disorders has been discussed for decades. Current research shows the connection is more complex than previously thought.
Dental issues like misaligned teeth or recent dental work may contribute to TMJ disorder, though evidence is mixed. A recent UK study found TMD symptoms in 20% of orthodontic patients. However, fixing bite alignment alone rarely resolves TMD completely, and unnecessary dental work can sometimes exacerbate symptoms.
Diagnosis
Getting an accurate diagnosis is essential for effective treatment. TMJ disorders can be complex, sometimes requiring several healthcare providers working together. Modern diagnostic techniques have improved in recent years, allowing for more targeted and effective treatment plans.
How is TMJ Disorder Diagnosed?
Diagnosing TMJ disorders requires a methodical approach combining clinical evaluation with patient history. Since there's no single test that confirms TMD, diagnosis often involves ruling out other conditions while building a complete picture of symptoms and jaw function.
Diagnosis typically involves:
- Medical History: Questions about symptoms, when they started, what triggers them, and lifestyle factors
- Physical Examination:
- Feeling the TMJ and facial muscles for tenderness
- Measuring how far the jaw can move
- Listening for joint sounds
- Checking bite alignment
- Imaging (if needed):
- X-rays: To detect bone problems or arthritis
- MRI: To see soft tissues like the articular disk
- CT scans: For detailed bone structure analysis
Can TMJ Symptoms Mimic Other Conditions?
Yes, TMJ disorder is often misdiagnosed because its symptoms overlap with:
- Ear infections (ear pain or pressure)
- Migraines or tension headaches
- Sinus problems (facial pain)
- Trigeminal neuralgia
- Dental problems like abscesses
This symptom overlap can delay proper diagnosis and treatment.
Treatment and Management
The good news about TMJ disorders is that simple treatments are often effective. Treatment approaches have changed in recent years, moving away from invasive procedures toward more holistic approaches that address underlying causes. Most patients can find relief without surgery.
At-Home Remedies
Self-care forms the foundation of TMJ treatment, with simple measures often providing substantial relief. These approaches are effective as initial steps or for managing mild cases without professional treatment.
- Ice/Heat Therapy: Ice for new inflammation (first 48 hours), heat for muscle relaxation
- Soft Foods: Temporarily switching to yogurt, soup, or soft foods to reduce jaw strain
- Jaw Exercises: Gentle stretching to improve mobility and strengthen muscles
- Relaxation Techniques: Mindfulness, meditation, or breathing exercises to reduce stress-related clenching
Medical Treatments
When self-care isn't enough, professional treatments offer additional options. TMJ care typically starts with minimal interventions before considering more complex treatments, allowing most patients to find relief without advanced procedures.
- Medications:
- Over-the-counter pain relievers (NSAIDs) for pain and inflammation
- Muscle relaxants for severe spasms (short-term use)
- Dental Interventions:
- Occlusal splints/mouthguards: Custom-fitted devices to reduce grinding and stabilize the jaw
- Dental adjustments: Correcting bite misalignment (though evidence is limited)
- Physical Therapy:
- Jaw exercises to improve mobility and strengthen muscles
- Manual therapy targeting the neck and jaw muscles
- Techniques like ultrasound or TENS for pain relief
- Advanced Treatments:
- Botox injections to relax overactive jaw muscles (50-70% effective in studies)
- Arthrocentesis: joint irrigation for severe cases
Do Bite Guards/Night Guards Really Help?
Yes, bite guards or night guards help 60-70% of TMD patients with grinding or muscle pain. Custom-fitted guards from dentists reduce clenching, protect teeth, and stabilize the jaw joint. They work best when combined with other therapies like stress management or physical therapy.
Is Surgery Common or a Last Resort?
Surgery is definitely a last resort, used in less than 5% of cases for severe, unresponsive TMD. Surgical options include arthrocentesis, arthroscopy, or open-joint surgery, but these carry risks of nerve damage or scarring. Current guidelines favor conservative treatments due to better outcomes and lower risks.
Is TMJ Disorder Permanent, or Can It Go Away?
The natural course of TMJ disorders varies considerably between individuals. Understanding typical patterns helps patients make informed decisions about treatment and maintain realistic expectations about recovery.
Many mild cases resolve within 1 to 2 weeks with self-care measures. Up to 40% of cases improve on their own without intervention. However, chronic cases may persist for months or years, especially in the absence of treatment for grinding or arthritis, necessitating ongoing management.
Can It Get Worse If Untreated?
Untreated TMD can potentially worsen, leading to:
- Chronic pain or central sensitization
- Permanent joint damage (cartilage erosion)
- Psychological distress (anxiety, depression)
- Progression from clicking to locking or limited movement
Is It Linked to Other Conditions?
TMJ disorders often don't exist in isolation but connect to other health conditions. Understanding these relationships can lead to more comprehensive treatment approaches that address underlying factors rather than just symptoms.
TMJ disorder is associated with:
- Arthritis (osteoarthritis or rheumatoid arthritis)
- Chronic pain syndromes (fibromyalgia, chronic fatigue)
- Psychological conditions (anxiety, depression)
- Sleep disorders
- Headache disorders
Frequently Asked Questions About TMJ Disorder
These common questions highlight areas of confusion about TMJ disorders. Understanding these basics can help you navigate both prevention and treatment more effectively.
What is the difference between TMJ and TMD?
TMJ refers to the temporomandibular joint itself, while TMD or TMJ disorder refers to the conditions affecting this joint and surrounding muscles.
Can children develop TMJ disorder?
Yes, though less commonly than adults. Children may develop TMD from habits like teeth grinding, jaw injuries, or orthodontic issues. Symptoms in children are often milder.
Is TMJ disorder hereditary?
There appears to be some genetic component. Studies show that TMD tends to run in families, suggesting genetic factors may influence susceptibility.
Conclusion
TMJ disorder can significantly impact quality of life, but most cases respond well to simple treatment. Understanding the symptoms and seeking timely care are key steps toward relief. If you're experiencing jaw pain, headaches, or any symptoms mentioned in this article, schedule an appointment with our clinic for proper evaluation and personalized treatment recommendations.






