Gum Disease: All You Need to Know
Noticed blood when brushing? It might be gum disease, a common issue that can lead to tooth loss and affect your health. Discover its causes, treatments, and easy ways to keep your gums healthy.

Imagine noticing a bit of blood on your toothbrush after brushing your teeth. It’s easy to dismiss, but this could be an early sign of gum disease, a common yet preventable condition that affects nearly half of adults and is a leading cause of tooth loss worldwide. Gum disease, ranging from mild gingivitis to severe periodontitis, impacts not just your smile but also your overall health, with links to heart disease and diabetes complications.
This blog provides a comprehensive guide to gum disease, covering its definition, symptoms, causes, diagnosis, treatment, complications, and prevention, all explained in clear, accessible language backed by scientific insights.
Let’s dive into what you need to know to protect your oral health.
What is Gum Disease?
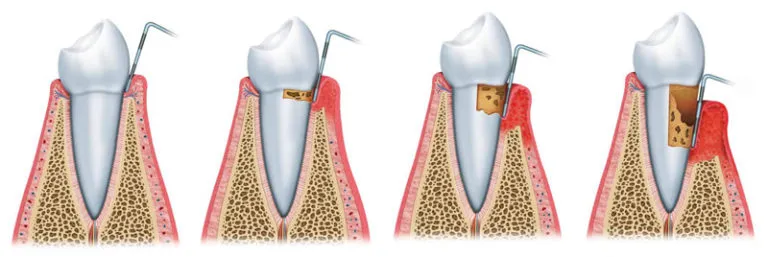
Gum disease, or periodontal disease, is an inflammatory condition affecting the periodontium: the gums, bone, cementum, and ligaments that support your teeth. It begins with gingivitis, a reversible condition characterized by gum redness and swelling, and can progress to periodontitis, a serious condition that damages the bone and tissues, potentially leading to tooth loss.
Gum disease affects 45% of UK adults, with 37% having moderate cases (gums with pockets 4–6 mm deep) and 8% facing severe cases (pockets 6 mm or deeper), based on the 2009 Adult Dental Health Survey. It’s more common as you age, hitting 53% for moderate and 11% for severe cases in people aged 65–74. Men (34% with moderate cases) and those with less education or living in poverty are at higher risk. Experts predict an 89% rise in cases by 2050, especially among older adults, as the population ages. The UK, Spain, Sweden, and Switzerland are the healthiest-ranked European countries in terms of low tooth loss and low prevalence of moderate to severe periodontal pocketing.
Types of Gum Disease
According to the 2017 EFP/AAP classification system, gum disease is categorized into three main groups: periodontal health and gingival diseases, periodontitis, and other conditions affecting the periodontium.
Periodontal Health, Gingival Diseases, and Conditions
- Healthy Gums: Picture healthy gums as a strong, snug collar around your teeth—no bleeding when you brush or floss, no loss of the tissue that anchors teeth (called clinical attachment loss, or CAL), and shallow pockets (≤3 mm) when a dentist measures the space between your gums and teeth. Even after successful treatment, gums can stay healthy with minimal redness or swelling, as long as no permanent damage occurs.
- Gingivitis (Caused by Plaque): This is when plaque—a sticky layer of bacteria from food and saliva—builds up and irritates your gums, making them red, puffy, and prone to bleeding when you brush. It’s like a skin rash that can be cleared up with proper care. With good brushing and flossing, gingivitis can be reversed, whether your gums are in their original state or slightly altered after treatment.
- Other Gum Conditions (Not Caused by Plaque): Some gum problems aren’t from plaque but from other issues, like autoimmune diseases (e.g., causing peeling gums, known as desquamative gingivitis), allergies, or injury (like burns from hot food). These can show up as sore, peeling, or ulcerated gums and need specific treatments depending on the cause.
Periodontitis
Periodontitis is the more serious form of gum disease, where inflammation damages the bone and tissues holding your teeth in place. The 2017 EFP/AAP system simplifies it into one category, moving away from older terms like “chronic” or “aggressive” periodontitis.
Think of periodontitis like a crack in your house’s foundation—it starts small but can worsen if ignored. The system uses stages (I–IV) to show how bad the damage is and grades (A–C) to predict how fast it might get worse, based on your health and habits:
Other Periodontal Conditions
- Necrotizing Periodontal Diseases: These are severe, painful conditions where gum tissue dies, forming ulcers between teeth, with heavy bleeding and bad breath. They’re often linked to stress, poor nutrition, or a weakened immune system, like a sudden, aggressive infection that needs immediate care.
- Periodontal Abscesses: These are painful pockets of pus in the gums, like a boil, that can destroy tissue quickly and, if untreated, spread infection to the rest of the body.
- Endo-Periodontal Lesions: These happen when infection from a tooth’s root (inside the tooth) and the gums connect, causing combined damage. It’s like two leaks merging into a bigger problem, needing careful diagnosis to plan treatment.
Gum disease is linked to systemic conditions like heart disease, stroke, and diabetes complications due to chronic inflammation, highlighting the importance of early intervention.
Symptoms of Gum Disease
Symptoms depend on the stage of gum disease:
- Gingivitis: Red, swollen, tender gums that bleed when brushing or flossing; bad breath or an unpleasant taste. T
- Periodontitis: All gingivitis symptoms, plus receding gums (making teeth look longer), deep pockets between gums and teeth (>3 mm), loose or shifting teeth, pus, pain when chewing, tooth sensitivity to cold, and bite changes.
- Acute Necrotizing Ulcerative Gingivitis (ANUG): Sudden, painful gum ulcers, severe bleeding, swelling, and bad breath.
- Desquamative Gingivitis: Peeling gums, often linked to conditions like Addison’s disease.
Dentists measure pocket depths and check for bone loss on X-rays to confirm severity. Early symptoms are often painless, so regular dental visits are crucial for catching issues before they worsen.
Causes and Risk Factors
The leading cause of gum disease is plaque, a sticky bacterial film that hardens into tartar, irritating gums, and causing inflammation. If left untreated, this leads to more severe tissue and bone damage. The oral microbiome can become imbalanced (dysbiosis), with harmful bacteria, spirochetes, and even rare protozoa like Entamoeba gingivalis contributing. Your immune system’s response can accidentally damage tissues further.
Risk factors include:
- Poor oral hygiene: Inadequate brushing or flossing allows plaque to build up.
- Smoking: Increases risk threefold and masks symptoms, making diagnosis more challenging.
- Hormonal changes: Puberty, pregnancy, or menopause can make gums more sensitive.
- Systemic conditions: Diabetes, HIV, Down syndrome, rheumatoid arthritis, and osteoporosis weaken immunity or bone health.
- Medications: Oral contraceptives, antidepressants, anti-seizure drugs, or angina treatments can cause dry mouth or gum changes.
- Other factors: Genetic predisposition, stress, low income, teeth grinding (bruxism), crowded teeth, poor nutrition (e.g., low vitamin intake), and rare causes like dental amalgam particles or Kaposi’s sarcoma.
Gum disease is also linked to systemic issues like heart disease, stroke, premature delivery (7.5x higher risk in pregnancy), and cancers (e.g., 49% higher risk for kidney cancer), though these connections are still being studied.
When to See a Dentist
Your gums are a window into your overall health, and even minor changes can signal the start of gum disease, which is why timely dental visits are critical for prevention and treatment. See a dentist immediately if you notice:
- Bleeding, tender, or swollen gums
- Persistent bad breath or taste
- Receding gums or loose teeth
- Pus between teeth or pain when chewing
Early detection can prevent gingivitis from progressing to periodontitis, often with just a professional cleaning. For advanced cases, your hygienist may refer you to a periodontal dentist for specific treatments, such as non-invasive periodontal treatment or further surgery if needed. Check-ups should not be more than 6 months apart, but occasionally sooner if we are concerned or if you have been categorized as high-risk. (e.g., smokers, diabetics).
Diagnosis of Gum Disease
Dentists use a combination of clinical assessments and specialized tools to evaluate the health of your gums and supporting structures, ensuring a tailored treatment plan. They will do a clinical examination, periodontal probing of your gums, dental radiographs and a medical history review.
How often do I need to come in for supportive periodontal treatment?
Every three months, it’s essential to clear away the bacterial biofilm that naturally builds up under the gums. If left untreated, this biofilm can irritate the surrounding tissues and trigger an exaggerated immune response, leading to further bone loss and disease progression.
Research shows that regular three-month maintenance significantly reduces the risk of flare-ups. When longer intervals are left between visits, maintaining a stable periodontal status becomes much less predictable, often requiring additional deep cleaning — and in some cases, even surgical intervention.
Treatment Options
Effective treatment of gum disease hinges on catching it early and tailoring interventions to its severity, from comprehensive cleanings to advanced surgical procedures, all aimed at halting progression and restoring oral health. Treatment varies by stage and diagnosis.
- Comprehensive cleaning above the gums and oral hygiene education
- Review of lifestyle factors, such as smoking cessation or control of factors like dry mouth resulting from medication or uncontrolled sugar levels.
- professional deep cleaning to tackle bacteria underneath the gums in deeper pockets
- Laser bacterial reduction
- Laser gingival contouring
- Resective or regenerative surgeries
- Removal of exacerbating factors, like replacement or repair of restoration,s which are causing food to adhere or get stuck. Occasionally, broken teeth or wisdom teeth need to be removed to improve the overall periodontal status.
- Platelet-rich fibrin (taken from venous blood in your arm) or local medicaments can be inserted into areas where bone loss has occurred to assist with regeneration and healing.
Quitting smoking, managing stress, and controlling conditions like diabetes support treatment success.
What periodontal care does Minty offer?
Periodontal disease currently has no cure, so regular assessment and maintenance are just as important as the initial treatment. At Minty, we’re committed to comprehensive periodontal care. Dr Nicole Betsis, who completed her MSc in Periodontology in 2018, stays at the forefront of modern periodontal therapies.
She is specially trained in advanced laser techniques that target inflammation, reduce harmful bacteria, and treat periodontal pockets — helping slow the progression of periodontal disease, including bone loss and tooth mobility.
We offer a range of minimally invasive, non-surgical treatments using laser technology. Where necessary, surgical therapies are also available for more advanced cases.
Complications of Untreated Gum Disease
Left untreated, gum disease can escalate from a minor annoyance to a serious health threat, impacting not just your mouth but your entire body, with consequences that affect both your quality of life and long-term health. Ignoring gum disease can lead to:
- Oral issues: Tooth loss, abscesses, tooth migration, and bite misalignment.
- Systemic risks: It’s linked by association to higher chances of heart attack, stroke, diabetes complications, premature delivery (7.5x risk), and cancers (49% kidney, 54% pancreatic, 30% blood). Bacteria may also worsen Alzheimer’s disease, although research is still ongoing.
- Social and economic costs: Difficulty chewing, aesthetic concerns, and costly advanced treatments.
Early action prevents these serious outcomes.
Prevention and Self-Care
Building a strong defense against gum disease starts with consistent daily habits and lifestyle choices that support healthy gums and overall wellness, empowering you to take control of your oral health. Protect your gums with:
- Daily hygiene: Based on your individual needs, your periodontist and dental hygienist will provide you with personalized oral hygiene guidance and home care recommendations.
The foundation of proper oral hygiene includes brushing twice daily for 2 minutes with a soft-bristle toothbrush (replace every 3 months) and flossing, using interdental brushes daily.
- Lifestyle:
- Quit smoking to boost treatment success.
- Eat vitamin C- and calcium-rich foods (e.g., oranges, yogurt); limit sugar.
- Manage stress with meditation or exercise to strengthen immunity.
- Stay hydrated to support saliva production, which fights bacteria.
- Dental visits: It is recommended to have dental check-ups and supportive hygiene care twice a year. However, patients at high risk for periodontal disease may require more frequent visits, as advised by their dentists..
- Monitoring: Watch for early signs, such as bleeding or swelling, and seek care promptly.

Special Populations
Certain groups, such as pregnant individuals, children, those with systemic diseases, or smokers, face unique challenges with gum disease due to biological, lifestyle, or health-related factors that heighten their risk or complicate treatment. Understanding these specific needs helps tailor prevention and care strategies to protect their oral and overall health effectively:
- Pregnant individuals: Hormonal changes increase gingivitis risk, and periodontitis may cause premature delivery or low birth weight. Regular dental care is vital.
- Children/teens: Rare aggressive periodontitis requires early treatment and parental supervision of brushing/flossing until age 8.
- Systemic diseases: Diabetes, HIV, or Down syndrome patients need regular check-ups and strict glycemic control to manage higher risks.
- Smokers: Smoking hides symptoms and reduces treatment efficacy, necessitating smoking cessation programs alongside dental care.
Conclusion
Gum disease is a preventable yet serious condition that affects your mouth and overall health. With nearly half of adults at risk, early detection through regular dental visits and consistent oral hygiene is crucial. Gingivitis can be reversed with simple steps, and even periodontitis can be managed with proper care. Schedule a dental check-up, take care of your oral hygiene at home daily, and tackle risk factors such as smoking or stress to protect your smile and well-being. With the right approach, you can keep gum disease at bay and enjoy a healthier life.