Gingivitis: Symptoms & Causes
Noticing red or bleeding gums? We’ll explore gingivitis, its symptoms, causes, and simple steps to prevent and reverse this common gum issue.

Gingivitis is the earliest stage of gum disease, affecting a significant number of people in the UK, and it's completely reversible with proper care. Understanding what causes gingivitis and recognizing its symptoms can help you take action before it progresses to more serious gum problems.
What is Gingivitis?
Gingivitis is inflammation of the gums caused by bacteria in plaque. When bacteria accumulate along your gumline, your body responds with inflammation, characterized by redness, swelling, and sometimes bleeding.
Think of gingivitis as an early warning system. It signals that something isn't right with your gum health, but no permanent damage has occurred yet. This distinguishes it from periodontitis, the advanced form of gum disease that damages the supporting structures of your teeth and can lead to tooth loss.
Gingivitis is extremely common. In the UK, studies show that more than 50% of adults have some form of gum disease, with gingivitis being the most prevalent type. Globally, estimates suggest that between 50-90% of adults worldwide experience gingivitis at some point in their lives. The variation in these numbers reflects differences in oral hygiene practices, access to dental care, and other factors across different populations.
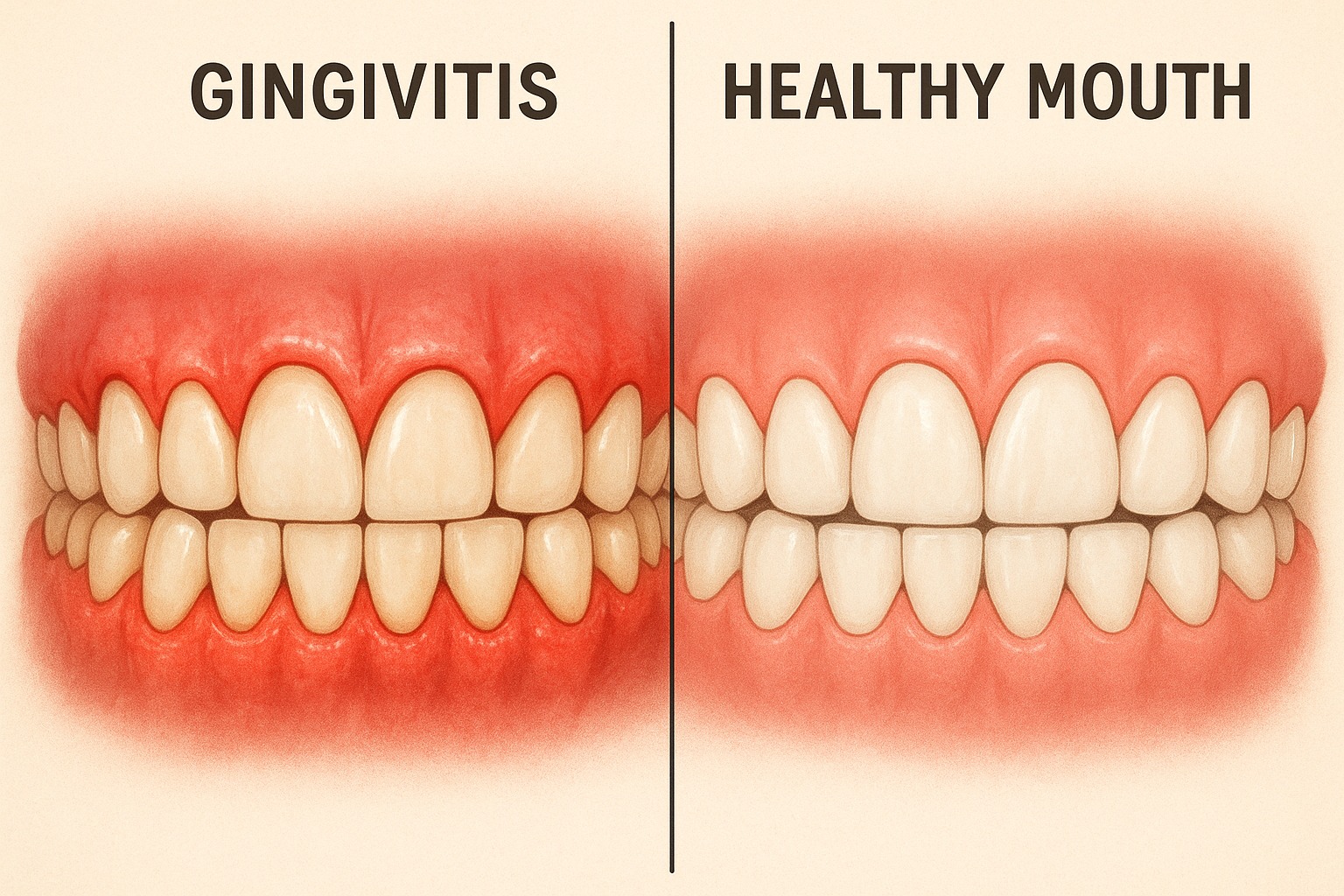
Healthy gums fit snugly around your teeth, are pale pink in color, and firm to the touch. With gingivitis, this changes as your body fights the bacterial infection.
Recognizing the Signs: Symptoms of Gingivitis
Many people have gingivitis without realizing it because early symptoms can be subtle. Here are the common signs to watch for:
Red or Swollen Gums
One of the first signs is a change in color. Healthy gums are pale pink, but infected gums become red or darker in color. They may also look puffy or swollen rather than firm.
Bleeding Gums
If your gums bleed when you brush or floss, this is usually abnormal. Even slight bleeding during oral care is typically a classic sign of gingivitis.
Tender Gums
Your gums might feel sore when touched or when chewing firm foods.
Bad Breath
Persistent bad breath that doesn't go away after brushing can indicate bacterial growth associated with gingivitis.
Receding Gums
In more advanced cases, your gums might start to pull away from your teeth, making your teeth look longer than before.
It's important to note that gingivitis often doesn't cause pain, which is why many people ignore the symptoms. However, painless doesn't mean harmless. Untreated gingivitis can progress to more serious gum disease.
Root of the Problem: What Causes Gingivitis?
Understanding what triggers gingivitis is the first step in preventing it. There's a complex battle happening in your mouth between bacteria and your body's defenses. Most causes are under your control, which means you can prevent and reverse this condition.
Plaque: The Primary Culprit
The main cause of gingivitis is dental plaque, a sticky, colorless film of bacteria that constantly forms on your teeth. Here's how it happens:
- After you eat, bacteria feed on food particles left on your teeth, especially sugars and starches.
- As they digest this food, they produce acids that irritate your gums.
- The bacteria multiply and form a biofilm (plaque) that clings to your teeth, particularly along the gumline.
- If not removed through brushing and flossing, plaque hardens into tartar within 24 to 72 hours.
- Tartar creates a shield for bacteria and can only be removed by professional cleaning.
The longer plaque and tartar remain on your teeth, the more they irritate the gingiva, the part of your gum around the base of your teeth. Your gums become inflamed, and gingivitis develops.
Beyond Plaque: Risk Factors That Increase Your Chances
While plaque is the direct cause of gingivitis, several factors can increase your risk or make the condition worse:
Poor Oral Hygiene
Inadequate brushing and flossing allow plaque to build up and harden into tartar.
Smoking and Tobacco Use
Smoking weakens your immune system and makes it harder for your gums to heal. Smokers are more likely to develop gum disease and often show fewer obvious symptoms like bleeding gums, which can
delay diagnosis.
Hormonal Changes
Fluctuations in hormones can make gums more sensitive and vulnerable to inflammation:
- Pregnancy ("pregnancy gingivitis")
- Puberty
- Menstrual cycles
- Menopause
Medical Conditions
Certain health issues increase your risk:
- Diabetes reduces resistance to infection and impairs healing
- HIV/AIDS weakens the immune system
- Blood disorders
- Autoimmune diseases
Medications
Some medications reduce saliva flow, which helps protect your mouth, while some cause abnormal gum tissue growth. Some examples are:
- Antidepressants
- Blood pressure medications
- Anticonvulsants (for epilepsy)
- Immunosuppressants
- Some contraceptives
Nutritional Deficiencies
Lack of vitamin C, which helps maintain healthy gums, can contribute to gum disease.
Crooked Teeth or Dental Appliances
Misaligned teeth, rough fillings, ill-fitting bridges, crowns, or dentures can create spaces where plaque accumulates more easily. This may be more difficult to clean, and in effect, can exacerbate gum disease.
Genetics
Some people are genetically more susceptible to gum disease, regardless of how well they care for their teeth.
Age
Risk increases with age, though gingivitis can affect people of all ages, including children.
The Gingivitis-Overall Health Connection
Research shows connections between gum disease and other health problems. The bacteria responsible for gingivitis can enter your bloodstream through inflamed gum tissue, potentially affecting other parts of your body.
Studies suggest links between gum disease and:
- Heart disease and stroke
- Diabetes (a two-way relationship where each condition can worsen the other)
- Respiratory diseases
- Rheumatoid arthritis
- Certain cancers
- Pregnancy complications
- Alzheimers and Dementia
The common thread appears to be inflammation. Chronic inflammation in your gums may contribute to inflammation elsewhere in your body.
While research continues, maintaining healthy gums appears to be increasingly important not just for your mouth, but for your overall health.

How Dentists Diagnose Gingivitis
Dentists diagnose gingivitis during regular check-ups by:
- Examining your gums for signs of inflammation
- Measuring the depth of spaces between your teeth and gums using a small probe
- Checking for easy bleeding
- Looking for tartar build-up
- Assessing your overall oral hygiene
Early detection is crucial in preventing more severe gum disease. This is why regular dental check-ups are crucial, even when you're not experiencing obvious symptoms.
Prevention Preview: Protecting Your Gums
Preventing gingivitis involves addressing the causes we've discussed. While we'll cover prevention in more detail in a future post, here are the essentials:
- Brush your teeth twice daily with fluoride toothpaste
- Clean between teeth daily with floss or interdental brushes
- Visit your dentist regularly for check-ups and professional cleanings
- Avoid tobacco products
- Maintain a balanced diet
- Manage conditions like diabetes that might affect your gum health
FAQs About Gingivitis
Is gingivitis contagious?
Gingivitis itself isn't contagious, but the bacteria that cause it can be transmitted through saliva. Whether someone develops gingivitis depends more on their oral hygiene practices and risk factors.
How quickly can gingivitis develop?
Gingivitis can develop within days to weeks of inadequate oral hygiene, though symptoms might not be noticeable immediately.
Can children get gingivitis?
Yes, children can develop gingivitis, especially during puberty when hormonal changes make gums more susceptible to inflammation.
Does gingivitis always lead to periodontitis?
No, not always. With proper treatment and improved oral hygiene, gingivitis can be reversed entirely before it progresses to periodontitis.
How long does it take to cure gingivitis?
With professional hygiene appointments as well as home care, gingivitis can often improve within a week or two. Maintaining good oral hygiene is essential to prevent it from returning.
Can stress cause gingivitis?
Stress doesn't directly cause gingivitis, but it can weaken your immune system and lead to neglect of oral
hygiene, both of which contribute to gum problems.
Are electric toothbrushes better for preventing gingivitis?
Some studies suggest electric toothbrushes remove plaque more effectively than manual brushes, but proper technique matters more than the type of brush. Either can be effective when used correctly.
Conclusion
Gingivitis is common but not inevitable. By understanding its causes and recognizing its symptoms, you can take steps to prevent it or seek treatment before it progresses to more serious gum disease.
Remember that healthy gums are the foundation of a healthy mouth, and potentially a healthier body. If you notice any signs of gingivitis, schedule a dental appointment. With professional care and improved home oral hygiene, gingivitis can be reversed, restoring your gums to health.






