Impacted Wisdom Teeth: Causes, Symptoms, and treatment
Jaw pain or swelling? Impacted wisdom teeth, stuck due to small jaws, can cause trouble. Learn the signs, causes, and treatments to keep your smile healthy and pain-free.

Long ago, our ancestors required strong jaws and extra teeth to chew through tough plants and raw meat. Now, our jaws are smaller, and for up to 90% of us, wisdom teeth (third molars) don’t have enough room to grow properly, leading to painful issues called impactions. An impacted tooth occurs when a tooth becomes stuck in the jawbone or gums. Approximately 1 in 4 people worldwide experience this condition.
This blog post serves as your friendly guide to understanding why wisdom teeth become impacted, the signs to watch for, and how modern dental care can help. If you’ve had wisdom teeth troubles or think you might, talk to a dentist and share your story in the comments.
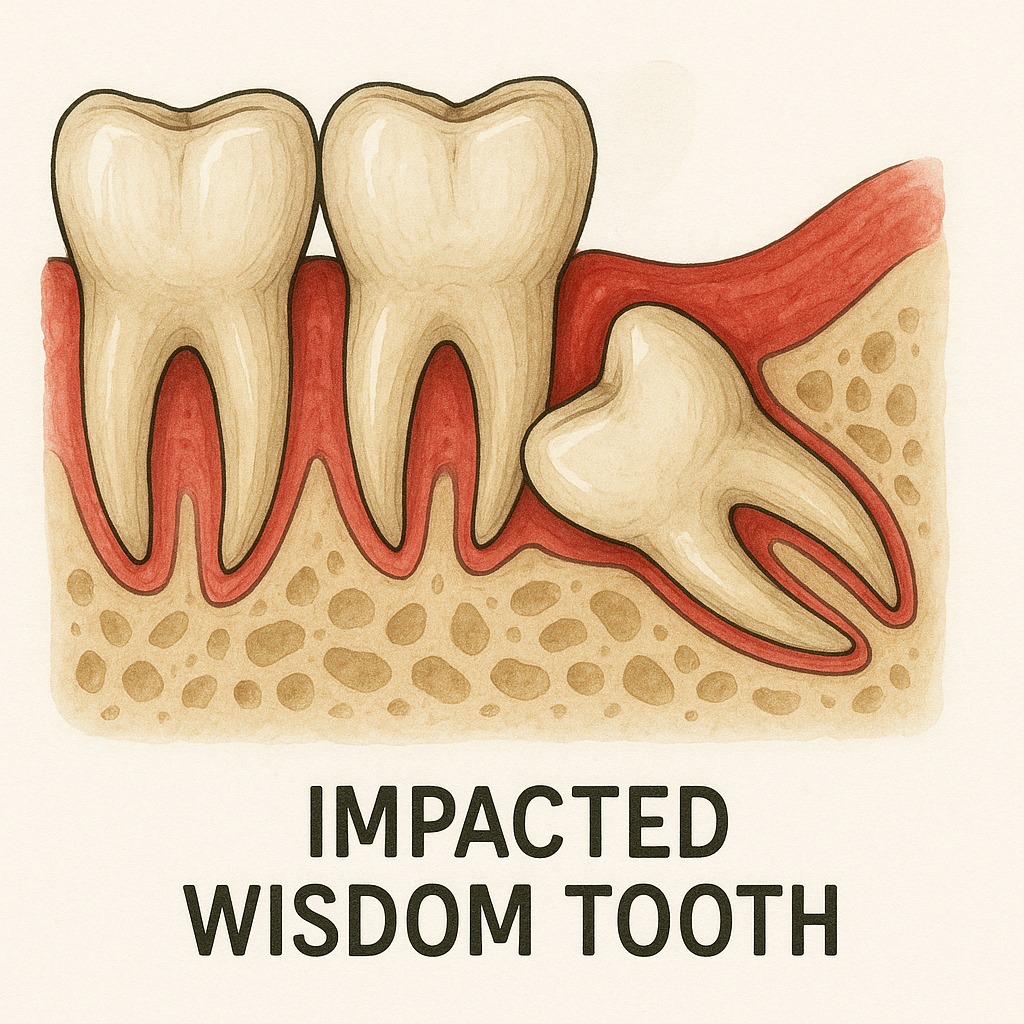
What Are Impacted Wisdom Teeth?
An impacted tooth is a wisdom tooth that can’t break through the gums because there’s not enough space or it’s growing at a wonky angle. These “third molars” usually show up between the ages of 17 and 25. They might be fully stuck in the jawbone or only partly out. They could be tilted toward nearby teeth, tilted backward, horizontal or in a vertical but tight (“crowded”) position.
If left unchecked, they can cause jaw pain and infections. That’s why seeing dentists early, ideally before age 24, is so important. A dental X-ray (panoramic radiograph) or a 3-dimensional CBCT (cone-beam CT scan) helps spot the problem and plan oral surgery if needed.
Why Do Wisdom Teeth Get Stuck?
Our jaws have shrunk over time because we eat softer foods compared to our ancestors, leaving less room for wisdom teeth. This is the main reason they get stuck. Other causes include:
- Not Enough Jaw Space: Our genes often give us smaller jaws, affecting 90% of people.
- Weird angles: Teeth can grow toward other teeth, backward, or even sideways, getting blocked.
- Family traits: Some folks inherit smaller jaws or don’t even have all their wisdom teeth (8% of people in the UK).
- Jaw Injuries: Accidents can change the jaw’s shape, making impaction more likely.

Signs of Impacted Wisdom Teeth
Impacted Wisdom Teeth can cause noticeable problems, but sometimes they’re silent, so regular dental visits are key. Common signs include:
- Jaw pain or swelling: Aching in your jaw or face, sometimes spreading to cause headaches.
- Red, puffy, or bleeding gums, often tied to pericoronitis (Infection) around half-out teeth.
- Bad breath or a bad taste, from food and bacteria getting trapped.
- Trouble opening your mouth or chewing comfortably.
Other signs you might notice:
- Earaches, from jaw pain spreading nearby.
- Swollen glands under the jaw, as your body fights infection.
- Ongoing headaches or sinus-like feelings, especially if upper wisdom teeth press near your sinuses.
- Crowding of other teeth, pushing them out of line, which might need orthodontics to fix.
Even without symptoms, wisdom teeth can harm nearby teeth in 30% of cases, so dental X-rays are crucial to check how they’re growing (tooth eruption).
How Are Impacted Wisdom Teeth Treated?
Treating impacted wisdom teeth depends on the symptoms, the tooth’s position, and your overall health. Here are the main options:
- Monitoring: If the teeth aren’t causing problems, Dentists may suggest regular check-ups with dental X-rays to watch for changes, especially for asymptomatic cases.
- Antibiotics for Infections: For pericoronitis or other infections, antibiotics can clear up swelling or pain, often paired with antiseptic rinses to clean the area.
- Tooth Extraction: The most common solution is removing the impacted tooth through oral surgery. Local anesthesia (“numbing the area”) keeps you comfortable, and an oral surgeon can handle complex cases, like teeth near nerves.
- Swelling and Pain Management: After surgery, dentists typically prescribe pain relievers and recommend using ice packs or saltwater rinses to reduce swelling and promote faster recovery and aftercare.
- Orthodontic Solutions: If crowding affects other teeth, orthodontics might be needed to realign your bite after extraction.
Early treatment can prevent complications, and dental insurance may cover part of the cost, depending on your plan. Always discuss options with your dentist to find the best approach for you.
Around the world, dental care differs: in the U.S., tooth extraction is often performed early on, whereas in the UK, guidelines suggest waiting unless there’s a problem. In some Asian cultures, wisdom teeth are viewed as a sign of maturity, so people may choose to delay treatment. These differences show how beliefs and healthcare systems influence dental choices.
What Can Go Wrong If Left Untreated?
If impacted wisdom teeth aren’t treated, they can lead to bigger issues:
- Infections: Pericoronitis, abscesses, or cellulitis can spread to your throat or cheek, needing antibiotics or quick care.
- Gum Flaps: A bit of gum (called an operculum) over half-out teeth traps food, thereby raising the risk of infection.
- Damage to Nearby Teeth: In 30% of cases, the second molar develops cavities or wears down, potentially leading to periodontitis (a stage of gum disease).
Oral Surgery, often with anesthesia (local and general), may be needed. Swelling and pain management helps during recovery and aftercare, but risks like dry socket (Alveolar Osteitis) or mandibular nerve (Nerve Injury Risk) (1–5% chance) mean you need a skilled clinician who can help maneuver these risks.
How Your Mouth’s Bacteria Play a Role
New research shows that bacteria in your mouth, like Porphyromonas gingivalis and Fusobacterium nucleatum, can make pericoronitis worse by growing in pockets around stuck wisdom teeth. These germs can even lead to infections that spread beyond your mouth. In the future, dentists might test your mouth’s bacteria to suggest special rinses or probiotics tailored to you. This link, found in a 2023 study, illustrates how your oral health impacts your overall well-being, making early care a prudent choice.
When to Visit a Dentist
Call a Dentist right away if you have ongoing Jaw Pain, Swelling, fever, or trouble swallowing. Regular check-ups and Dental X-rays by age 16–18 help track Tooth Eruption. Ask your Dentist:
- What happens if I wait to treat this?
- Could my mouth’s bacteria affect my treatment?
Should You Remove Wisdom Teeth?
The American Dental Association (ADA) and the UK’s NICE guidelines (updated since 2000) suggest not removing Wisdom Teeth if they’re not causing trouble, to avoid risks such as nerve damage. However, a 2018 study and a 2025 X survey (where 68% of Dentists support early removal) indicate that leaving them can harm nearby teeth in 30% of cases. Your age, health, and tooth position matter.
Take Charge of Your Dental Health
Impacted wisdom teeth happen because our jaws are smaller than our ancestors’, leaving no room for teeth that grow at odd angles. They can cause Jaw Pain, Swelling, Bad Breath, or even rare issues like cysts. Getting checked early, ideally before age 24, can prevent problems like Pericoronitis or damage to nearby teeth. Talk to a Dentist or Oral Surgeon for advice tailored to you.






